Understanding the Concept of Do Not Resuscitate (DNR) in Terminal Patients: Ethical and Medical Practice Perspectives
[easy_youtube_gallery id=TbN0UbEDCPA cols=1 ar=16_9 thumbnail=0 title=top]First Video[/easy_youtube_gallery]
Presentation of Raboan material by dr. Lucia.Yogyakarta, 19 February 2025 – As part of the Raboan: Research and Perspective Sharing series, a discussion was held on the topic The Concept of Do Not Resuscitate (DNR) Orders in Terminal Patients with DPJP”. The event featured dr. Lucia Pudyastuti Retraningtyas, SpA., M.Bio.Et, a lecturer at the Faculty of Medicine, Universitas Surabaya, as the keynote speaker. The discussion was moderated by drg. Agnes Bhakti Pratiwi, MPH, Ph.D., from the Center for Bioethics and Medical Humanities (CBMH), Faculty of Medicine, Public Health, and Nursing (FKKMK), Universitas Gadjah Mada, as well as the UNESCO Chair on Bioethics at UGM.
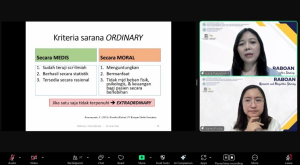
This webinar highlighted various perspectives on DNR orders for terminal patients. DNR is a medical decision made by the medical team after consulting with a team appointed by the Medical Committee or Ethics Committee. Ideally, the decision-making process should involve both the patient and their family. Communication between the patient, family, and healthcare providers is crucial in identifying the patient’s values, preferences, and critical medical care decisions. dr. Lucia emphasized that DNR orders must be clearly documented and recorded in the patient’s medical records.
Discussion Session With Participant
One key point discussed was the importance of respecting patient dignity in end-of-life care. Physicians have different perspectives on DNR orders, with some agreeing and disagreeing them. Reasons for agreeing DNR Orders : reducing patient suffering and ensuring a peaceful passing; alleviating the burden on the family during the patient’s final moments, facilitating the work of other medical personnel in providing appropriate care; religious considerations that align with end-of-life dignity; legal aspects that support the implementation of DNR. Reasons for disagreeing DNR Orders: concerns over family misconceptions and potential conflicts; the belief that doctors must provide the maximum possible care to every patient; fear of causing family distress or uncertainty regarding medical decisions.
DNR is also linked to the Sustainable Development Goals (SDGs), particularly: SDG No. 3: Good Health and Well-Being, which emphasizes the importance of access to quality healthcare services, including palliative care and the patient’s right to decide on end-of-life care. SDG No. 10: Reduced Inequalities, which highlights that every patient has the right to make medical decisions without pressure or discrimination, including decisions regarding DNR orders.
This Raboan discussion reaffirmed that a bioethical approach to implementing DNR orders is essential in end-of-life nursing and medical decision-making. Through effective communication between doctors, patients, and families, it is hoped that medical decisions can be made ethically and in alignment with human values.
Reporter : Ardhini Nugrahaeni,M.K.M
Editor : Alvira Rahmasari, S.H.G.







Leave a Reply
Want to join the discussion?Feel free to contribute!