Bridging the Gap: Uncovering Health Inequities and Moving Forward
Yogyakarta, June 18, 2025 – Raboan Research and Perspective Sharing returned with a highly relevant and thought-provoking topic: “Ethics in the Distribution of Catastrophic Health Services under BPJS.”
This session featured expert speaker Prof. dr. Laksono Trisnantoro, M.Sc., Ph.D., Professor at the Department of Health Policy and Management, Faculty of Medicine, Public Health, and Nursing (FMPHN), Universitas Gadjah Mada. The discussion was moderated by Mahmasoni Masdar, S.Kep., Ns., M.Kep from CBMH UGM. Together, they explored the pressing issue of inequality in access to healthcare services across Indonesia.

Drawing from BPJS data from 2015 to 2023, Prof. Laksono presented how advanced medical procedures such as cardiac catheterization (Cathlab) remain concentrated in Java and Bali. In contrast, eastern regions like Papua and Maluku are significantly underserved. This disparity raises an ethical concern, as all BPJS members—regardless of their backgrounds—deserve equal access to life-saving health services.
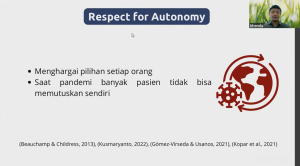
Prof. Laksono also introduced ethical frameworks based on Pareto efficiency and Rawlsian justice in public policy, prompting reflection with questions such as: Is it justifiable that only a portion of the population benefits from state-of-the-art healthcare, while others lack even basic referral access? Is it ethical to allow a system to continue operating without addressing deeply rooted structural inequalities? As stated in the Pareto principle:
“A policy is considered good if at least one group becomes better off, without making others worse off.”
Raboan session was highly interactive, with participants from various professional backgrounds calling for true implementation of equity and social solidarity within the National Health Insurance (JKN) system.

This theme strongly aligns with the Sustainable Development Goals (SDGs), especially SDG 3: Good Health and Well-Being and SDG 10: Reduced Inequalities. Equal access to catastrophic health services is not merely about equipment or budgets—it is a matter of dignity and justice for all Indonesian citizens.
This Raboan discussion reaffirmed that equitable access to healthcare is not merely a matter of infrastructure and funding, but a question of justice and human dignity. It is hoped that this forum will serve as a concrete impetus for policymakers to build a more just, inclusive, and people-centered health system for all Indonesians.
[easy_youtube_gallery id=Iqs3kioSJR4 cols=1 ar=16_9 thumbnail=0 title=top]Etika dalam Pemerataan Pelayanan Kesehatan Katastropik BPJS[/easy_youtube_gallery]

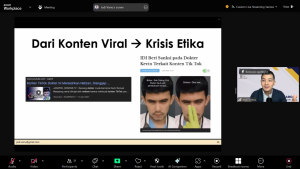


 “As medical professionals, our duty is not only to provide medical benefits, but also to ensure that our actions are fair and respect the rights of patients,” said dr. Wikan.
“As medical professionals, our duty is not only to provide medical benefits, but also to ensure that our actions are fair and respect the rights of patients,” said dr. Wikan.