Center for Bioethics and Medical Humanities Universitas Gadjah Mada (CBMH UGM) held its regular Raboan event with the theme “Family Decision Making” on Wednesday, October 8, 2024. The event was hosted via Zoom and featured Lintang Sagoro, MD, a master’s student from Harvard Medical School, as the speaker. The webinar was attended by students, academics, and healthcare practitioners interested in medical ethics and policy issues.
Lintang Sagoro, MD, opened the discussion by highlighting the crucial role of the family in decision-making for the care of patients with serious illnesses. “Medical decisions are not just about the therapies to be administered, but also about how to maintain the quality of life of the patient, both physically and emotionally,” he explained. Lintang Sagoro, MD emphasized that honest and transparent communication between patients, families, and healthcare providers is essential for ensuring the well-being of the patient, especially in the context of palliative care.

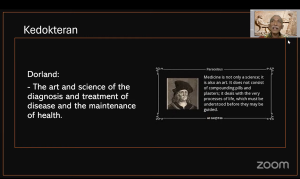
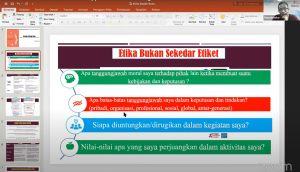
In the first session, Lintang Sagoro, MD discussed the importance of bioethical principles in medical decision-making, grounded in the values of Pancasila. The concepts of respect, beneficence, and justice, which advocate for the respect of all forms of life, including humans, animals, and the environment, serve as the foundation that must be considered in every medical decision. “The principle of patient autonomy must be balanced with family responsibility, and we need to ensure that decisions reflect the noble values that underpin bioethics,” he said.
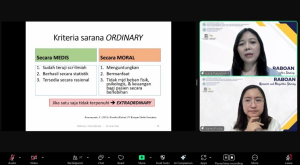
The discussion then moved to the topic of palliative care, which aims to improve the quality of life for patients with serious illnesses. Lintang Sagoro, MD explained that palliative care is not meant to replace curative treatment, but rather to complement it by focusing on the comfort of the patient, as well as providing emotional and spiritual support for both the patient and their family.

Communication challenges between families and patients were also a key point of focus in this webinar. Lintang Sagoro, MD revealed that families often face dilemmas in disclosing the health condition of patients with severe illnesses, as they try to protect the patient from stress that may arise from unpleasant information. “It is important for healthcare providers to help families deliver information carefully and empathetically, so the decision-making process can proceed smoothly,” he said.
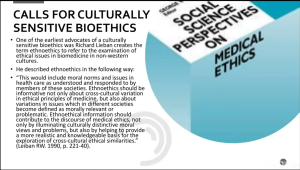
The webinar also highlighted the cultural differences in medical decision-making between Indonesia and Western countries. In Indonesia, medical decisions tend to involve the extended family, whereas in countries like the United States, patient autonomy plays a more dominant role in determining their care. This difference underscores the importance of understanding cultural context in medical practice.
The discussion was relevant to SDG 3 on Good Health and Well-Being, which emphasizes the importance of quality and inclusive healthcare. Family-based decision-making and honest communication in the care of patients with serious illnesses support efforts to achieve better access to holistic palliative care. This also contributes to reducing healthcare inequities and enhancing the well-being of both patients and families facing difficult conditions.
At the conclusion of the event, Lintang Sagoro, MD encouraged participants to better understand the importance of emotional support for families caring for patients with serious illnesses, as well as the need to integrate palliative care into the healthcare system. “Support for caregivers is crucial, as they not only care for the physical needs of the patient, but also face significant emotional challenges,” he remarked.
For more information, please visit the official of CBMH UGM
E-mail : cbmhfkugm@ugm.ac.id
Youtube : CBMH UGM
Instagram : cbmh_ugm
Reporter : Alvira Rahmasari, S.H.G.
Editor : Rafi Khairuna Wibisono, S.Kom.






Follow us